For most people, bar those who have lost loved ones or continue to struggle with symptoms, the Covid-19 pandemic has faded into insignificance. We are no longer living in an active pandemic, and so it seems a bit over the top to continue worrying about Covid.
There is frequent mention of new variants, but it is exhausting to try and follow every update, especially when most of these new variants bring little change.
But recently, there has been some concern around the latest one – the Eris variant, named after the Greek goddess of strife and discord.
This new variant has arrived in South Africa and the South African Medical Association (SAMA) has cautioned, in an article on the Citizen website, that the strain could cause severe symptoms for those who are immune compromised and people who are over 65 and not vaccinated.
So, should you be worried? Do you need to find your face masks once again?
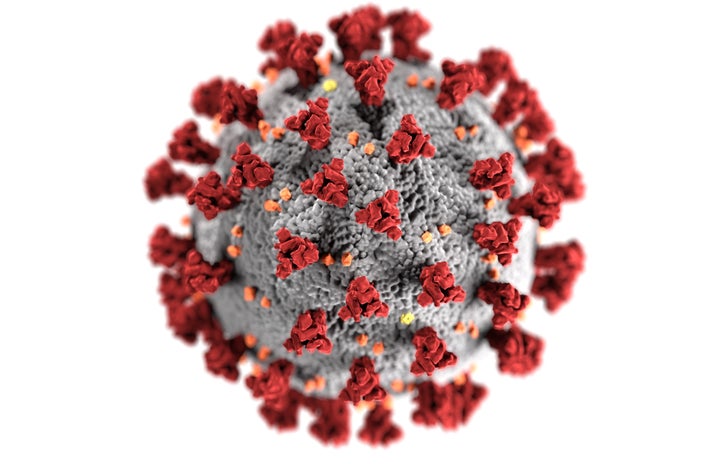
The Eris variant is also known as EG.5. This alphanumerical name is just a way of classifying new variants scientifically, based on how they have changed from the previous variant, and how they have evolved from the original strain of the SARS-CoV-2 virus, which caused the Covid-19 pandemic.
When a virus mutates, its genetic makeup is altered to allow the new variant to function slightly differently from the previous version. In the case of viruses affecting humans, such as coronaviruses, this often means that the new variants will be slightly more infectious, but are unlikely to cause more severe illness.
It might seem counterintuitive, but it is quite logical for a virus to mutate away from causing severe disease. This evolutionary strategy helps the virus to ensure its own survival. Because viruses cannot survive without a host, it makes sense for a virus to evolve to become more transmittable and thereby infect more hosts. However, if the virus causes an infection so severe that it kills off its host, the virus itself will also die out, as it will eventually run out of hosts to infect.
Unsurprisingly, this is exactly the case for the Eris variant: it has a higher rate of transmission. In other words, it spreads more easily from one person to another. Luckily, the World Health Organisation (WHO) says there is no evidence that Eris is any more severe than previous variants. It is unlikely to cause hospitalisation in younger people who do not have a compromised immune system, and most people who do test positive will be able to recover at home within a few days.
Gavi, the Vaccine Alliance, has confirmed that Eris is an offshoot of Omicron, as with most variants emerging now. Gavi is a partner of the WHO, the World Bank and Unicef.
Omicron was a variant that emerged in late 2021. It caused major concern, as it led to a much higher number of mutations in comparison to the Covid strains that it had evolved from. But despite many genetic differences, Omicron did not drastically increase the severity of Covid-19 cases. While higher case numbers did prove it to be more infectious, hospitalisations did not hugely increase.
Eris is similar – while it may be more infectious, it does not necessarily cause severe disease. This means that although more people may test positive for Covid, and cases may start to rise again, the Eris variant is unlikely to cause many deaths.
If you are up to date on your vaccines, and you are neither old nor immunocompromised, you don’t need to be overly concerned. Those who are immune compromised, however, might not fight off infections as well as other people, as their immune system is weaker than it should be.
This means that immunocompromised people are often more susceptible to infectious diseases than the rest of the population. While immunocompromised people can receive the mRNA Covid-19 vaccines, these vaccines have varying efficacy in immunocompromised populations. This means that not only are immunocompromised people more at risk of these diseases, but they may also have less chance of protecting themselves from infection. For this reason, it falls on the rest of the population to protect these individuals. This is known as “herd immunity”. If a large enough proportion of a population is vaccinated against a disease, the threshold of immunity in that population will be great enough to prevent the disease from spreading amongst the population. In this way, vulnerable members of that population will be protected against infection, even if they themselves are not vaccinated.
But there is one key caveat: herd immunity requires enough of the “herd” to actually be vaccinated. In this era of so much misinformation about vaccines and the growing anti-vaccine movement, it may be difficult to reach the level of vaccine uptake required for herd immunity, leaving immunocompromised people at risk.
The mRNA Covid-19 vaccines are still effective against the Eris variant. If you are not yet vaccinated but would like to be, or if you would like a booster vaccine, you can find your closest vaccination site on the South African Covid-19 Online Resource and News Portal, at https://sacoronavirus.co.za/.
The WHO has raised concern at the fact that too many people in vulnerable populations have not recently received another Covid-19 vaccine. Immunity afforded by the vaccines may wane over time, so if you have been told to get a booster, it is a good idea to follow through.
If you are infected with Eris, it is best to stay at home until you have recovered. The symptoms of Eris are similar to previous Covid variants, including a runny nose, fever, fatigue, cough, sore throat, and changes in smell or taste.
So, in summary, most of us who are vaccinated and who are not immunocompromised probably don’t need to be too worried about the Eris variant. But keeping your vaccinations up to date for the sake of the herd is important, and will ultimately help you to protect yourself as well.